Endocrine Surgery
30+ Years of surgical experience
Warning
If you have any of the below problems and have not been checked for the specified endocrine cause, you should consult an endocrinologist.
- Arrow Brittle and painful bones and urinary stones may be due to excess parathyroid hormone.
- Fluctuating blood pressure and anxiety attacks may be due to adrenal and other neuroendocrine tumors.
- Fits and episodes of unconsciousness when hungry, may be due to an insulinoma rather than a form of epilepsy.
- Acidity and persistent or recurrent stomach ulcers may be due to gastrinoma.
- Obesity may be due to Cushing’s disease or thyroid deficit.
- Weight loss may be due to excess thyroid.

Thyroid swelling (Goiter)

What are the causes of Goiter?
Thyroid swelling can be due to tumors, iodine deficiency, autoimmune (self destructing) conditions, infection, etc.
What are the ill effects of Goiter?
Thyroid swellings can compress the vital structures under it like the gullet, breathing tube, speech nerves, etc. causing difficulty in swallowing, breathing, speech, etc.
There may be excessive or decreased production of thyroid hormone.
If there is cancer it can spread and produce problems in other parts of the body.
How do you test a Goiter?
Ultrasound scan, FNAC (Fine Needle Aspiration Cytology), Thyroid function tests, Anti thyroid antibodies assay etc. are done. When required, Radio isotope scan, CTscan of neck and chest, MRI scan, blood tests for cancer markers may be done.
How is a Goiter treated?
Depending on the cause it is treated with appropriate medicines, radioactive iodine and surgery to remove the whole thyroid (Total Thyroidectomy) or half of it (Hemi Thyroidectomy) or part of it (partial/ subtotal Thyroidectomy/ lobectomy/ Isthumusectomy).
What are the types of anesthesia and surgery for Goiter?
Thyroid surgery can be done under local, regional or general anesthesia, with a 7 to 10cm cut across the neck by open surgery or when feasible through a small less than 3 cm skin cut by endoscopic (minimally invasive) surgery.
What are the risks of thyroid surgery?
Possible risks include: 1) bleeding that can cause acute breathing difficulty, 2) hoarseness due to injury to the speech (recurrent laryngeal) nerve, and 3) damage to the parathyroid glands that control calcium levels in the body, causing hypoparathyroidism. The overall risk of complications should be <2% with an experienced surgeon.
What can I do before thyroid surgery to be optimally prepared?
It is important that you do not eat or drink anything after midnight the night before surgery. Continue to take all important medications such as heart, asthma, or blood pressure medicines as advised by your anesthesiologist with a small sip of water on the morning of surgery. Diabetic medicines are not taken by mouth on the day of surgery. Do not take blood thinning drugs or aspirin for 7-10 days prior to your surgery date. Quit smoking.
Will I have pain? Will I have stitches? What can I expect after surgery?
You will be asleep during your surgery and will feel no pain. Pain after surgery is easily suppressed by prescribed medicines. Stitches placed under the skin are not visible and dissolve after a period of time and do not need to be removed. You might have a sore throat, difficulty swallowing, or a slightly hoarse voice after the operation. These conditions will resolve with time. There may be a tube (surgical drain) in the incision in your neck (which will be removed the morning after the surgery). Once you are fully awake, you will be moved to a bed in a hospital room where you will be able to eat and drink as you wish. Most patients having thyroid operations are hospitalized for about 24 to 48 hours. Near normal activity can begin on the first day after surgery. You will have some difficulty with full range of movement of your neck for one week after surgery. You can return to work in 1-2 weeks time. Vigorous sports should be delayed for at least 1 month. You may experience low blood calcium (hypocalcaemia). You may need to take Thyroid hormone (Thyroxin) tablets, calcium and vitamin D after surgery, sometimes lifelong. During your follow-up visit, your TSH (thyroid stimulating hormone) levels will be checked and Thyroxin dose adjusted accordingly.
What are the signs of low blood calcium and how will I know if I need to take extra calcium?
Low blood calcium occurs if the parathyroid glands (behind the thyroid gland) do not function properly. Symptoms of low blood calcium include numbness and tingling in the fingers and around the mouth, weakness, headaches, muscle cramps, intestinal cramps, heart arrhythmia (rhythm disturbance). Low blood calcium can be prevented or treated with extra calcium intake. Left untreated, very low calcium levels can cause chocking.
Will I have a scar?
All surgeries cause some scarring. When performed by skilled endocrine surgeons, the thyroid operation will be performed using the smallest, cosmetically placed incision possible. Plastic surgery type closures are used to minimize scarring. Ultimately the type of scar formed depends mostly on the type of your body response to any injury. The majority of people having thyroid surgery have minimal scar present by 6 months after surgery
How is thyroid cancer treated?
It is treated by surgery to remove the entire thyroid (Total Thyroidectomy) and certain adjoining tissues (depending on the type of cancer and extent of spread). This is followed by radioactive ablation (RAI) i.e. destruction of any residual thyroid or cancer with radioactive isotope of iodine as Iodine is preferentially taken up by thyroid tissue from the blood stream. Thyroid hormone (Thyroxin) tablets have to be taken daily, life-long. Regular check up (may include scans, blood tests for TSH, Thyroglobulin, calcitonin, etc.) is essential to detect any recurrence early.
What is the outlook or prospects (prognosis) for patients with thyroid cancer?
The outlook for patients with thyroid cancer is excellent in that safe and effective therapy is available in most cases. Even those patients whose thyroid cancer cannot be cured, can usually live a long time and feel well despite their cancer.
Parathyroid Swelling (Adenoma, Hyperplasia, Carcinoma) - Hyperparathyroidism
What is Parathyroid?
Parathyroids are four tiny glands hidden near the thyroid gland in the neck. They produce and release parathyroid hormone which controls the calcium levels throughout the body. Excess production of parathyroid hormone (PTH) by abnormal parathyroid gland(s) is called Hyperparathyroidism
What happens in Hyperparathyrodism (parathyroid excess)?
Kidney stones, bone pains, bone cysts and swellings, joint swellings, peptic ulcer pain made worse by antacids, weakness, fatigue, and depression can be due to hyperparathyroidism.
How do you test for it?
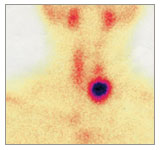
This can easily be detected by checking blood for serum calcium and PTH (Para thyroid hormone),both of which will be abnormally high. It can then be localized by ultrasound scan and Technetium Tc 99m Sestamibi scan
Why is treatment important?
Left untreated bones become weak and break easily. Kidney stones keep growing and reforming after removal, ultimately damaging the kidneys.
How is Hyperparathyroidism treated?
Treatment requires surgical removal of the abnormal parathyroid gland(s). Usually there is a single parathyroid adenoma and it needs to be identified and removed (Parathyroidectomy). Occasionally there may be more and these need to be detected and removed. Sometimes one adenoma is dominant, and other adenomas may become obvious later.
If there is hyperplasia, all glands except half a parathyroid gland are removed. It is preferable to transplant this half into an easily assessable muscle in the neck or forearm so that if it grows excessively, parts of it can be removed easily.
For parathyroid cancer, the adjacent half of the thyroid gland is removed (Hemi Thyroidectomy) in addition to the parathyroid cancer.
If there is hyperplasia, all glands except half a parathyroid gland are removed. It is preferable to transplant this half into an easily assessable muscle in the neck or forearm so that if it grows excessively, parts of it can be removed easily.
For parathyroid cancer, the adjacent half of the thyroid gland is removed (Hemi Thyroidectomy) in addition to the parathyroid cancer.
What are the types of anesthesia and surgery for parathyroid adenoma removal?
Parathyroid surgery can be done under local, regional or general anesthesia.
Traditionally a large 7 to 10cms cut is made across the neck and the entire front side of the neck is searched for these four tiny parathyroid glands by an experienced surgeon. The Technetium Tc 99m Sestamibi scan (a radio-isotope scan) has revolutionized the identification and treatment of abnormal parathyroid glands. The use of this radio-isotope scan and the ultrasound scan has made minimal surgery possible for parathyroid adenoma. There are many methods of minimally invasive/ endoscopic surgery for the removal of parathyroid adenoma. These techniques (totally endoscopic, video assisted and radio guided) have been demonstrated to be feasible and safe, but it depends on the surgeon to obtain the best results with these approaches. The surgery can be done through a single cut less than 3 cm or through three to four 5mm cuts in the armpit and breast. A specialist endoscopic & endocrine surgeon (a rare species!) would be conversant with all the open and endoscopic methods and offer you all the possible options. ENT/ Head & neck surgeons, surgical oncologists, general surgeons, laparoscopic surgeons also operate on the parathyroid gland(s), each by the method they are familiar with.
Complications are rare under the expert care of an experienced endocrine surgeon. The success of the procedure can be determined soon after and the patient is fit to go home in a few hours though we advise our patients to stay till the calcium levels stabilize a bit.
Will I have pain? What can I expect after surgery?
Mild pain after surgery is easily suppressed by prescribed medicines. You might have a sore throat, difficulty swallowing, or a slightly hoarse voice after the operation. These conditions will resolve with time. Once you are fully awake, you will be moved to a bed in a hospital room where you will be able to eat and drink as you wish. Near normal activity can begin on the first day after surgery. You may have some difficulty with full range of movement of your neck for a week after surgery. You can return to work in a few days time but be careful with your brittle bones. Vigorous activities and sports should be delayed as the bones weakened by the parathyroid problem take time regaining there strength. You may experience low blood calcium (hypocalcaemia). You will need to take calcium and vitamin D tablets. During your follow-up visit, your Calcium levels will be checked and medication dose adjusted accordingly.
What are the signs of low blood calcium and how will I know if I need to take extra calcium?
Symptoms of low blood calcium include numbness and tingling in the fingers and around the mouth, weakness, headaches, muscle cramps, intestinal cramps, heart arrhythmia (rhythm disturbance). Low blood calcium can be prevented or treated with extra calcium intake.Left untreated, very low calcium levels can cause chocking.
Insulinoma & Neuro endocrine tumors

What is Insulinoma?
Insulinoma is a tiny insulin hormone producing tumor in the pancreas, an organ for digestion located behind the stomach. The excess insulin hormone dangerously lowers the blood sugar levels. This is the opposite of diabetes where there is an insulin deficit and high blood sugar.
How does it manifest?
A desire to eat frequently, and stomach discomfort when hungry followed by sweating, dizziness, confusion and even fits and loss of consciousness may be due to an insulinoma rather than a form of epilepsy. These symptoms can be avoided by frequent snacking and are relieved by glucose.
How do you test for it?
The insulinoma can be easily diagnosed by checking blood during such an episode or after a few hours of starvation. The blood sugar will be very low and the insulin level high.These tumors are less than 15mm (1/2 inch) in size and hence difficult to locate. Various sophisticated scans, etc.,are used to locate these tiny tumors.
How is it treated?
In most hospitals a major part of the pancreas is removed surgically as the insulinoma is too small to be identified by an inexperienced surgeon. As Pancreas is a very important organ for both digestion and preventing diabetes, every effort should be made to conserve it. A well defined insulinoma can be easily removed without sacrificing the pancreas provided it is identified. We are able to identify and specifically remove such an insulinoma even by laparoscopic surgery so that the patient recovers rapidly and returns to normal activity. If an insulinoma is not well defined we localize it by the various sophisticated methods listed earlier. We have pioneered a method of conserving the pancreas even in such patients. This kind of minimal pancreas surgery avoids converting a person from a state of excess insulin (insulinoma) to a state of severe insulin deficit (labile diabetes) which is difficult to manage. Complications are uncommon under the expert care of an experienced surgeon.
Sometimes the problem may not be localized (Nesidioblastosis) and a part of the pancreas may have to be removed by open surgery. Only about 10% of these tumors are cancers and need extensive removal followed by anti cancer medication.
What about Neuro endocrine tumors other than Insulinoma?
Other Neuroendocrine tumors (a rare, distinct group) include: Gastrinoma, Glucagonoma, Somatostatinoma, VIPoma, Carcinoid, etc.
Most of them have fairly similar characteristics in spite of the different hormones made by them. These similarities include symptoms like diarrhea, sweating, anxiety, headache, fatigue etc.
Gastrinoma is tiny like an insulinoma and the same tests are used to locate it. Unlike other islet cell tumors it often occurs outside the pancreas especially in the duodenum (initial part of small intestines). The surgery for it is similar to that for insulinoma except that it involves an extensive search even outside the pancreas.
The tumors other than Gastrinoma are usually large. Most are cancers requiring extensive surgery and additional treatments like hormone therapy, chemotherapy, biologic therapy (immunotherapy), etc.
Adrenal Tumors (Pheochromocytoma, Conn’s syndrome / aldosteronOMA, Cushing’s syndrome and Incidentalomas)
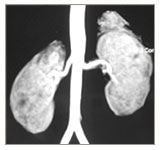
What are Adrenal glands?
A thumb sized, triangular shaped adrenal gland is located on the top of each of the two kidneys. They produce hormones adrenaline, aldosterone and cortisol. These hormones maintain salt and water balance, control blood pressure, stress responses, and some sexual functions.
How does an adrenal growth manifest itself?
High blood pressure, headache, palpitations, anxiety, weakness, fatigue, cramps, tingling sensation, weak bones (osteoporosis), Diabetes, overweight-obesity, infertility,streaks on the abdomen, acne and facial hair, can be caused by adrenal tumors.
How do you detect an Adrenal tumor?
Ultrasound, CT, MRI scans can detect adrenal tumors. The tumor is identified by testing urine and blood for the hormones (and byproducts) produced by it. Sometimes Isotope and PET scans or selective venous sampling may be required to localize them.
How is the tumor removed?
Surgical removal of the adrenal gland is called adrenalectomy. This is best done by Laparoscopic Surgery, thus facilitating early recovery and return to normal activity. Large tumors are removed by Hand Assisted Laparoscopic Surgery or conventional open surgery. Sometimes laparoscopic adrenalectomy is not possible due to various factors and the surgeon may decide on open surgery either before or during the actual operation. There are many ways of approaching the adrenal in both laparoscopic & open surgery. The backside and side approaches are easier and faster but have certain constraints. The front approach is tedious but provides many more options. A specialist endoscopic (laparoscopic) & endocrine surgeon (a rare species!) would be conversant with all these methods and approaches and these technicalities are best left to the specialist surgeon to decide. Urologists, surgical oncologists, general surgeons, laparoscopic surgeons also operate on the adrenals, each by the method they are familiar with. Complications are rare if adequate preparations are done and precautions taken under the expert care of an experienced endocrine surgeon.
